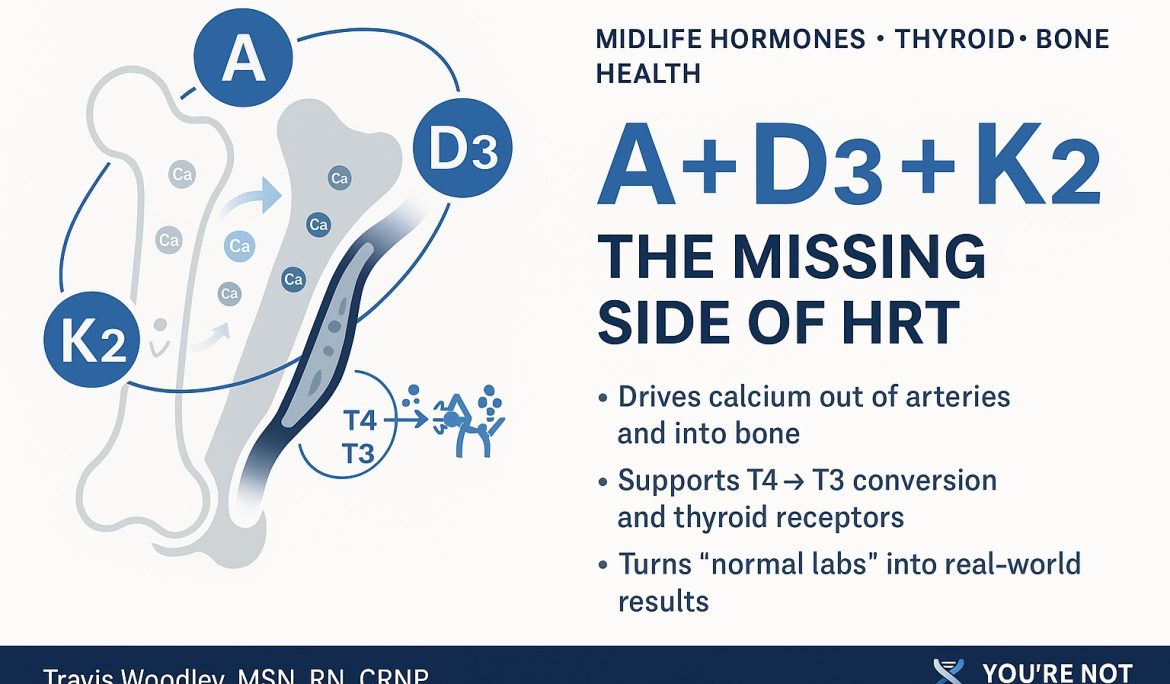
The Most Overlooked Trio in Midlife Health: Vitamin A, D3, and K2
Vitamin A, D3, and K2 are not “nice add-ons” to a supplement stack—they are the traffic controllers for calcium, thyroid conversion, and hormone receptors.
When ADK is ignored, you can lift, diet, take bioidentical hormones, and still harden arteries, stall metabolism, and feel half-alive with “normal” labs.
That sounds dramatic, but this is exactly what I see every week in practice.
Midlife men and women are often doing a lot of things right:
-
They’re on hormone replacement.
-
They’ve cleaned up their nutrition.
-
They’re lifting weights and walking.
-
Their labs are “optimized.”
And yet they’re still exhausted, inflamed, frustrated with their weight, and worried about bone density or cardiovascular risk.
A big reason: no one has ever talked to them about the quiet power of vitamin A, D3, and K2.
Calcium Is Always Moving – The Question Is Where?
Your body is constantly deciding where to park calcium:
-
In bone and teeth – where you want it for strength and structure
-
Or in arteries, heart valves, joints, thyroid, and breast tissue – where it becomes a long-term problem
That choice is strongly shaped by three vitamins:
-
Vitamin D3 – increases absorption of calcium and interacts with immune and hormone target cells
-
Vitamin K2 – activates proteins that escort calcium into bone and keep it out of soft tissues
-
Vitamin A – helps build the receptors and proteins that allow hormones and thyroid signals to do their job
When ADK is dialed in, calcium is used to reinforce the skeleton and support healthy signaling.
When ADK is ignored, calcium can slowly accumulate in the wrong places—while bones still don’t get the full benefit.
D3 and K2: The “Where Does Calcium Go?” Problem
Most people have heard about vitamin D. Very few have heard a meaningful conversation about vitamin K2.
Here’s the simple map I use with patients:
-
Vitamin D3
-
Increases calcium absorption from the gut
-
Influences bone remodeling cells (osteoblasts and osteoclasts)
-
Interacts with immune cells and hormone target tissues
-
-
Vitamin K2
-
Activates vitamin K–dependent proteins, especially:
-
Osteocalcin – helps lock calcium into bone matrix
-
Matrix Gla Protein (MGP) – one of the strongest protectors against calcium hardening arteries and soft tissues
-
-
When you load up on D3 and never address K2, it’s like turning on a firehose with no one directing the spray. You absorb more calcium, but you don’t fully control where it ends up.
Over time, that can mean:
-
Bone density that looks better on paper,
-
While arteries and soft tissues pay the price in the background.
This is part of what’s often called the “calcium paradox”: you can have calcium deficiency in bone at the same time you have excess calcification in soft tissues.
K2 is one of the keys to resolving that paradox.
Vitamin A: The Quiet Architect of Hormone and Thyroid Signaling
Vitamin A doesn’t get nearly enough attention in hormone and metabolic conversations.
It’s not just about “eyesight” or “skin health.” Vitamin A is deeply involved in:
-
Hormone receptor function
-
Thyroid hormone conversion and sensitivity
-
Immune regulation and mucosal barrier integrity
1. Hormone Receptors
Testosterone, estrogen, progesterone, thyroid hormone, and vitamin D all signal through nuclear receptors—proteins that sit on DNA like light switches.
Vitamin A (through retinoic acid) and vitamin D share partnering receptor systems. If A and D are off, the “switches” don’t flip cleanly.
What that means in real life:
-
Hormones are present in the bloodstream
-
Labs look “optimal”
-
But the signal at the DNA level is blunted
That’s how you end up with someone who is “optimized” on paper and still feels wrecked.
2. Thyroid Conversion: T4 → T3
Most thyroid hormone produced is T4—the storage form.
For your cells to actually use it, T4 has to convert to T3, the active form, primarily in the:
-
Liver
-
Gut
-
Peripheral tissues
That conversion relies on:
-
Deiodinase enzymes
-
Healthy liver and gut function
-
Adequate vitamin A, vitamin D3, iron, selenium, zinc
When vitamin A and D are off, you can see:
-
“Normal” TSH
-
“Normal” free T4
-
Suboptimal T3 and/or sluggish receptor response
Clinically, this looks like:
-
Cold hands and feet
-
Fatigue and low motivation
-
Constipation or slow digestion
-
Weight that will not move despite effort
-
Brain fog and lower mood
And the person keeps hearing, “Your thyroid is normal.”
No—that lab panel is conventional. The physiology is not.
ADK + BHRT: Why Labs Are Not the Whole Story
This article is about ADK—but it’s impossible to talk about midlife health and ignore hormone replacement and metabolic repair.
When we use bioidentical hormone replacement (BHRT), we’re asking the body to:
-
Rebuild bone and preserve muscle
-
Support cognitive function and stable mood
-
Improve insulin sensitivity and metabolic health
-
Restore libido and sense of vitality
All of that is calcium- and receptor-dependent work. It relies on:
-
Calcium going to the right tissues
-
Thyroid signaling and conversion functioning smoothly
-
Hormone receptors being responsive and ready
If ADK is ignored while we push hormones and nudge thyroid, we can unintentionally create this pattern:
-
Bone density improves on a scan
-
Arteries and soft tissues slowly stiffen
-
Muscle and strength gains underperform the hormone dose
-
Thyroid and sex hormone labs “look great”
-
The patient feels maybe 20–30% better—but not like themselves
In my Rebuild Metabolic Health framework and in my book, You’re Not Broken – You’re Unbalanced, I do not treat hormones, thyroid, micronutrients, gut, and immune as separate projects.
They are one signaling network.
What I See When ADK Is Off
Patterns I commonly see when vitamin A, D3, and K2 haven’t been addressed:
-
Long-term D3 supplementation with no K2 and a history of calcium-based supplements
-
“Osteopenia” or “osteoporosis” diagnosis despite years of standard “bone support”
-
Normal or high D levels, but persistent fatigue, brain fog, and joint pain
-
Thyroid labs that are technically “in-range,” with classic hypothyroid symptoms
-
Perimenopausal or andropausal patients on BHRT who say,
“I feel better than I did, but I still don’t feel like me.”
Once we correct ADK and integrate it with hormone and metabolic work, I consistently see:
-
Better bone and muscle changes for the same hormone dose
-
Calmer joints and less “mysterious” inflammation
-
More stable energy, mood, and mental clarity
-
Less of the “I’m doing everything and still not getting there” frustration
Where to Start
A few principles you can discuss with your clinician:
-
Stop thinking of vitamin D in isolation.
If you’re taking D3, there should be a conversation about K2 and, ideally, vitamin A status and overall micronutrient health. -
Think in systems, not single numbers.
-
Hormone replacement
-
Thyroid function
-
ADK status
-
Gut and liver health
-
Immune and inflammatory tone
All of these feed into the same outcomes: how you feel, how you age, and how well your metabolism responds.
-
-
Use quality, medical-grade formulations when possible.
Not all ADK products are created equal. Purity, dosing, and the presence of synergistic nutrients (like magnesium) matter for both safety and effectiveness. -
Work with someone who understands both hormones and micronutrients.
You deserve more than, “Your labs are fine.” You deserve someone who can explain why you feel the way you do and how these systems connect.
Important: Nothing here is personal medical advice. It’s a framework. Your doses, labs, and treatment decisions should always be guided by a qualified clinician who knows your full history.
If You’re Tired of Feeling “Normal” but Not Well
A big part of my mission—as a clinician and as an author—is to help people understand they’re not broken, they’re unbalanced.
ADK is a perfect example of that:
You’re not broken because your bones are thinning, your energy is low, or your metabolism is stubborn.
You’re living in a system that has been treated in pieces instead of as a whole.
When we step back and rebuild the entire signaling environment—hormones, thyroid, gut, immune, and key micronutrients like A, D3, and K2—people stop just surviving midlife and start actually feeling like themselves again.
Go Deeper with the Full Framework
If this resonated with you and you want the bigger picture on hormones, metabolism, peptides, thyroid, gut, and real-world midlife repair, I unpack the full roadmap in my book:
📘 You’re Not Broken – You’re Unbalanced
-
Purchase on Amazon: https://www.amazon.com/Youre-Not-Broken-Youre-Unbalanced-rebuilding/dp/B0FQJNQ6XP/ref=tmm_pap_swatch_0
-
Purchase on multiple platforms: https://books2read.com/Youre-not-broken
🧪 Medical-Grade Supplements & Peptides (Including ADK Support)
If you’re looking for high-quality formulations that align with the principles in this article and in the book, you can find them here:
📨 Resources, Articles & Newsletter
🎥 Follow & Connect
-
Instagram: https://www.instagram.com/yourenotbrokenofficial/#
-
Subscribe on LinkedIn newsletter: https://www.linkedin.com/build-relation/newsletter-follow?entityUrn=7385386886221074432
This is the kind of conversation I believe needs to become standard in midlife medicine—because you’re not broken. You’re unbalanced. And that can be rebuilt.