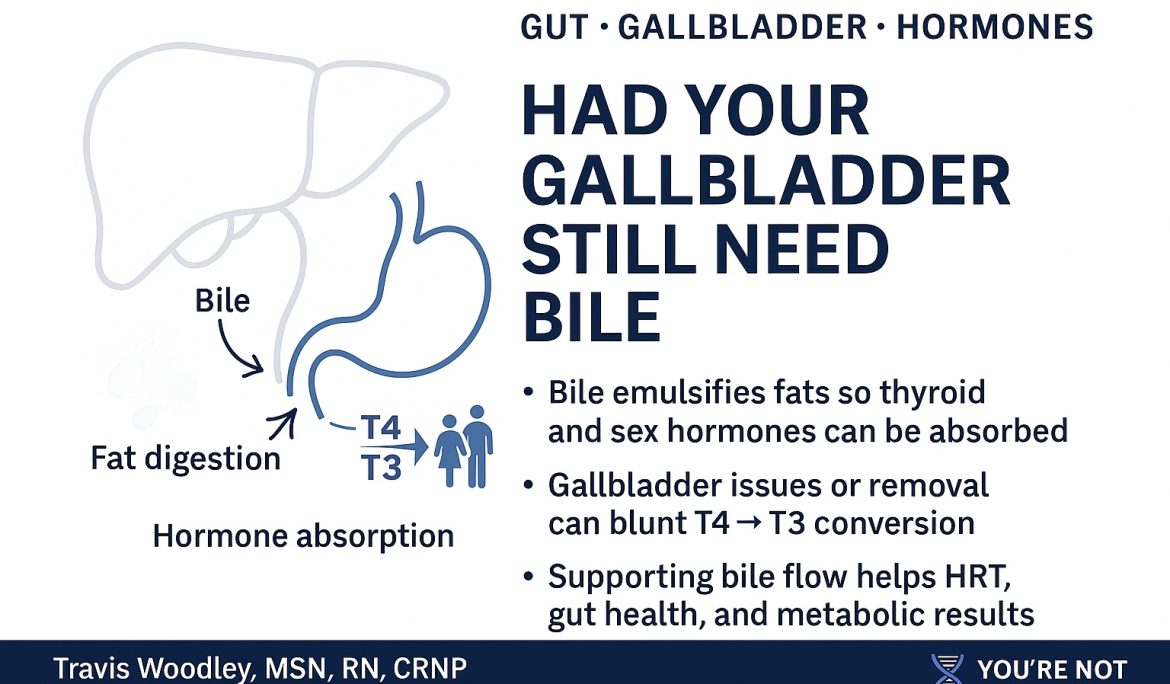
Your gallbladder may be small, but it’s one of the most ignored hormone and metabolism organs in the body.
We talk endlessly about thyroid, estrogen, testosterone, GLP-1s, and gut health… while forgetting the structure that decides what happens to every bite of fat you eat and every fat-soluble hormone signal that rides along with it.
When the gallbladder is sluggish—or removed entirely—you don’t just “lose a storage pouch.”
You change:
-
How you absorb essential fats and fat-soluble vitamins
-
How you convert T4 → T3
-
How you clear estrogen and other hormones
-
How your microbiome, bile acids, and metabolic signaling work after every meal
That’s not a side note. For many of my midlife patients, it’s the missing chapter.
The gallbladder: a metabolic control valve, not just a “sack of bile”
The liver is constantly making bile. The gallbladder concentrates and times its release.
When you eat a normal-fat meal, a healthy gallbladder contracts in a sharp, coordinated pulse. That pulse:
-
Emulsifies dietary fats so pancreatic lipase can actually break them down
-
Delivers bile acids into the small intestine, where they act as signaling molecules, not just detergents
-
Helps escort cholesterol, toxins, and hormone metabolites—especially estrogen—out of the body
If bile flow is thick, sluggish, or poorly timed, or if the gallbladder has been removed, you lose that control valve. Instead of precise pulses, you get a slow leak of dilute bile that rarely matches what you’re eating.
That’s where hormone, gut, and metabolic trouble start to stack up.
Bile acids: where digestion meets hormones
Bile acids do far more than digest fat. They act like hormones themselves, binding to receptors such as FXR and TGR5 on cells in the gut, liver, brown fat, and immune system.
Through those receptors, healthy bile signaling can:
-
Modulate insulin sensitivity and glucose handling
-
Influence GLP-1 and other gut hormone release
-
Affect mitochondrial function and energy expenditure
-
Help maintain a healthier balance of gut microbes
Now layer hormones on top of that:
Estrogen and bile
-
Estrogen is conjugated in the liver and sent out in bile for removal.
-
Sluggish bile flow or chronic bile stasis makes it easier for conjugated estrogen to be de-conjugated by gut bacteria and reabsorbed.
-
Clinically, this can look like “estrogen dominance” symptoms—breast tenderness, heavy cycles (if still cycling), fluid retention, and mood swings—even when labs are “in range.”
Thyroid and bile
The liver and gut are major sites for T4 → T3 conversion. When bile flow is impaired:
-
Fat-soluble nutrients (A, D, E, K, essential fatty acids) are less available to support thyroid receptors and immune balance.
-
Inflammation and dysbiosis in the small intestine can impair deiodinase activity, making it harder to convert T4 to active T3.
-
Patients may have “normal” TSH and T4 with persistent fatigue, weight gain, constipation, and cold intolerance—because the downstream conversion and receptor function are compromised, not just the gland.
Sex hormones and bile
-
Testosterone and progesterone metabolism depend heavily on hepatic clearance and bile excretion.
-
Poor bile flow can contribute to a picture where labs look acceptable, but tissues are living in a higher-estrogen, lower-androgen environment: lower lean mass, more visceral fat, lower libido, flatter mood, and poorer insulin sensitivity.
This is why I don’t treat midlife hormone replacement as “estrogen/testosterone in, job done.” If bile isn’t moving, those hormones won’t behave the way you and I want them to.
What actually happens when the gallbladder is sluggish?
Common patterns I see in clinic:
-
Early fullness, nausea, or “I just can’t tolerate fatty foods”
-
Bloating and right upper quadrant discomfort after meals
-
Floating, greasy, or difficult-to-flush stools (classic maldigestion of fat)
-
Worsening cholesterol despite “doing everything right”
-
Increased reflux as poorly digested food sits longer in the stomach and upper small bowel
Under the surface, there’s usually a combo of:
-
Incomplete fat digestion → more undigested fat reaching the colon, feeding dysbiosis
-
Reduced absorption of vitamins A, D, K2, and E
-
Subtle changes in thyroid conversion and estrogen clearance
-
Higher inflammatory tone and more oxidative stress at the hepatic and gut level
Give that system GLP-1 agonists, oral hormones, or an ultra-processed diet, and it often tips from “compensating” into full-blown symptoms.
What if the gallbladder is gone?
After cholecystectomy, the liver still makes bile—but you lose the concentrated, meal-timed release.
Common realities no one explains well:
-
Bile drips continuously into the intestine, often too little when you’re eating, and too much when you’re not.
-
Many patients unconsciously drop fat intake because it “tears up my stomach,” which further starves hormone pathways of needed building blocks.
-
Chronic, lower-grade fat malabsorption can quietly erode vitamin A/D/K status, bone density, and hormone receptor health over years.
These are the patients who often show up in my office with:
-
History of gallbladder removal 5–10 years ago
-
Gradual weight gain, fatigue, joint aches
-
Perimenopause or menopause symptoms that feel “out of proportion” to labs
-
New or worsening IBS-type complaints
If we only chase estrogen, progesterone, and testosterone numbers and never address bile physiology, we’re treating their labs, not their actual biology.
Supporting bile, hormones, and metabolism with and without a gallbladder
This isn’t medical advice for your specific case, but here’s how I think through support in my practice.
If you still have a gallbladder
Goals: improve bile quality, contraction, and timing; reduce inflammatory load; protect the liver.
-
Nutrient-dense, real food as a baseline: high-quality protein, non-starchy vegetables, strategic whole-food fats (olive oil, avocado, cold-water fish, egg yolks if tolerated).
-
Adequate—but not fear-driven low—fat intake. Chronically low-fat diets can worsen bile stasis because the gallbladder never fully contracts.
-
Bitters and bile movers (food-based): arugula, dandelion greens, lemon, ginger, beets—these can help stimulate bile flow in many people.
-
Targeted digestive support when appropriate: a comprehensive formula that includes bile salts, lipase, and pancreatic enzymes can help emulsify fats and reduce post-meal nausea, bloating, and greasy stools.
-
Magnesium and fiber to keep motility moving so conjugated hormones aren’t sitting in the colon waiting to be reabsorbed.
-
Attention to hormones themselves: Bioidentical hormone replacement (when indicated) should be dosed and delivered with the liver in mind. Transdermal routes and physiologic dosing are often friendlier to hepatic clearance than aggressive oral strategies.
If your gallbladder has been removed
We can’t replace the organ, but we can support the physiology it used to manage.
Key levers:
-
Consistent, moderate fat per meal (instead of huge high-fat boluses or extreme low-fat eating). This gives the liver a predictable workload.
-
High-quality digestive support with each meal:
-
Bile salts and ox-bile derivatives
-
Lipase and other pancreatic enzymes
-
Sometimes added taurine or glycine to support bile conjugation
-
-
Routine monitoring and replacement of fat-soluble vitamins (A, D, K2) and omega-3s, especially in midlife women on BHRT or struggling with bone density and thyroid symptoms.
-
Aggressive gut support when needed: protecting the ileum and colon from chronic fat irritation, reducing small intestinal bacterial overgrowth risk, and maintaining healthy bowel patterns.
When we get this right, patients without a gallbladder often tolerate a healthier, more metabolically appropriate diet again, and their hormone replacement stops feeling like “pushing on a locked door.”
Why gallbladder and bile physiology matter in BHRT and metabolic medicine
In You’re Not Broken – You’re Unbalanced, I talk about how midlife symptoms show up when systems drift out of sync—thyroid, sex steroids, insulin, circadian rhythm, and the gut-immune axis.
The gallbladder and bile network sit right at the crossroads of those systems:
-
They decide whether your BHRT actually reaches receptors in a healthy, anti-inflammatory environment
-
They determine whether your thyroid conversion is supported or constantly swimming upstream
-
They shape the microbiome signals that talk to GLP-1, leptin, and brain centers for appetite and mood
-
They influence whether “normal labs” translate into real-world resilience, body composition, and brain clarity
When we don’t ask about gallbladder history, post-cholecystectomy symptoms, or bile-related red flags, we miss a major reason someone’s hormones “don’t work” the way the textbook promised.
Bringing it together
If you’re a patient:
-
Your history of gallbladder attacks, sludge, stones, or removal is not an incidental footnote.
-
If you’re on hormone replacement and still feel exhausted, inflamed, foggy, or bloated—your bile and digestive signaling deserve as much attention as your lab ranges.
-
Work with a clinician who is willing to look at the whole system: liver, gallbladder (or lack of it), bile physiology, gut, thyroid, and hormones as one connected conversation.
If you’re a practitioner:
-
Ask about gallbladder history before you escalate hormone doses or add another metabolic drug.
-
Think beyond “fat digestion” and consider bile acids as endocrine and immunologic signals.
-
Remember that many midlife patients are navigating perimenopause, prior cholecystectomy, GLP-1 use, and decades of ultra-processed food at the same time. Their physiology is more complex than a single receptor.
This is the kind of systems-level work we do every day at Rebuild Metabolic Health Institute and in my clinic. When you treat the gallbladder–bile–hormone axis with the respect it deserves, midlife health stops feeling like a slow unraveling and starts to look like something you can actively rebuild.
If you want to go deeper into how hormones, gut, and metabolism actually interact in real people—not just in lab values—you can explore more in my book You’re Not Broken – You’re Unbalanced and the resources below:
-
Purchase the book on Amazon: https://www.amazon.com/Youre-Not-Broken-Youre-Unbalanced-rebuilding/dp/B0FQJNQ6XP/ref=tmm_pap_swatch_0
-
Purchase the book on multiple platforms: https://books2read.com/Youre-not-broken
-
Browse medical-grade supplements, including digestive and ADK support: https://www.revitalizenutrition.net/shop-now#!/Youre-Not-Broken-Medical-Grade-Supplements/c/186608296
-
Resources & newsletter: https://rebuildmetabolichealth.com/